Shepherd Village's proaction save lives
June 8, 2020
With a population of nearly 900 seniors, Shepherd Village is Toronto’s largest service retirement community.
Yet, they remain unscathed as there have been no active cases of COVID-19 that has ravaged long-term care homes in the Greater Toronto Area.
Just two residents and a similar number of staff tested positive.
What is noteworthy is that they contracted the virus outside the eight-and-a-half acre community.
Shepherd Village offers four types of accommodation – retirement & assisted living, rental apartments, life lease residences and long-term care.
There are 252 beds in the seven-story long-term care home.
Wendy Beckles, the President & Chief Executive Officer, said a resident in the long-term care home tested positive while he was hospitalized.
“This individual has underlying medical conditions and we had to send him to hospital because we can’t handle the acute care side of things,” she said. “This particular resident was back and forth between our facility and the hospital over the course of a few months. We tested him when he was with us and the hospital tested him when he was with them. Whenever he came back to us, he was isolated for 14 days. This is done with every resident that has to go to a hospital and our staff wear their full PPE (Personal Protective Equipment) when they are interacting with those in quarantine.”
Another resident in an independent apartment also tested positive during a hospital visit. She was bed-ridden.
“Everyone that took care of her including a daughter tested negative,” said Beckles. “We are thinking she must have got it in the ambulance or in hospital.”
The independent apartments contain 500 residents, many of whom go to grocery stores and banks.
“We call family members to help them, but invariably they have to go and the stores don’t allow them to bring their little carts anymore,” Beckles said “Sometimes, they have to go at least three times a day to the grocery store because they can’t lift more than one bag at a time. It’s tough.”
The two staff members were tested after complaining of feeling sick.
“The procedure is that once someone isn’t feeling well and depending on the symptoms, our infection control lead will direct them to be tested, “ Beckles noted. “When they came back positive, we immediately did a nasal swab of all the residents and staff on the floor that would have interacted with the two positive workers. All the results came back negative.”
With the novel coronavirus outbreak starting in Wuhan, China last December and Shepherd Village located in a Scarborough area with a high Asian population, Beckles acted immediately.
Shepherd Village in Scarborough
In early January, Shepherd Village started taking proactive measures by establishing a COVID Preparedness Team to ensure the virus didn’t infiltrate its community.
“It is clear that no one in long-term care would have been adequately prepared for this pandemic,” she said. “Having said that, it came down to how soon processes and procedures were implemented together with the intensity and consistency of our efforts. We started off in January by restricting access to the Village and a few weeks later, we closed our doors to visitors. Only staff and essential visitors, who initially were allowed entry to see family members in palliative care, were allowed in and they were all screened. Just one family member was allowed in at a time for an allotted period. At the same time, staff was restricted to work on one floor which is what we do whenever there is an outbreak. They weren’t even allowed to leave for lunch. You come to work and you bring your lunch to prevent the back and forth.”
Asking staff to choose one employer was another important preventative step Beckles and her management team took.
To make ends meet, many Personal Support Workers (PSW) work in more than one-long term care home. Even before the pandemic, the industry was struggling to recruit PSWs in particular because of the low pay, heavy workload and the abuse many suffer at the hands of seniors.
In mid-April during the pandemic peak, Ontario Premier Doug Ford issued an emergency order prohibiting employees from working at multiple facilities to slow the spread of COVID-19.
“We started the discussion long before the government issued that order and the idea was to keep our doors closed,” Beckles pointed out. “For the staff coming in, we recognized we had to educate them by letting them know they should reduce their social activities in the community and how to properly wear their masks and PPEs.”
Prior to the government order, Shepherd Village lost about 20 per cent of its nearly 460 full and part-time staff.
“By the time the provincial mandate came out, some staff started having child care issues, there were a few with immune systems that are compromised and others had seniors at home to care for,” Beckles said. “That lifted the level of staff we lost to 30 per cent. All of this was happening at a time when we had to have more screeners and people to assist our residents with FaceTime or Zoom so they could communicate with families through these social media platforms. The cleaning and sanitization throughout our community also took up hundreds of hours.”
The day after the World Health Organization (WHO) declared the coronavirus outbreak a pandemic on March 11, Shepherd Village rolled out its pandemic plan.
“Every day during the week and sometimes on weekends, I meet with my management team at 9.30 in the morning to go over everything, including any directive that may have come out in the last 24 hours, what are the implications and how are we following up,” said Beckles. “Before that, our Preparedness Team was meeting weekly, saying this thing is coming and let us get ahead of it.”
As frontline staff quit their jobs and long-term care homes struggled to find PSWs, Beckles remained confident that her facility wouldn’t be hit with a severe staff shortage in the middle of a pandemic.
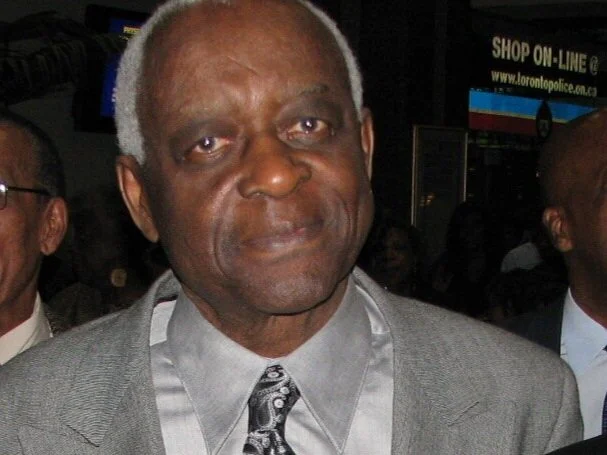
“We started hiring and we built trust and invested in our staff,” the 2019 Harry Jerome Award recipient said. “They saw we were providing PPEs and we weren’t waiting until the government announced emergency funding. I already had approval from my Board to re-allocate capital reserves because I had to purchase supplies and hire people. I am sure this sent a message to our staff that management was looking out for us. The staff stepped up and have worked beautifully as a team in these challenging times. I am very proud of them.”
Cognizant that families are eager to visit long-term care homes to see their loved ones, Beckles said that is a top priority.
“It’s a step, however, that we have to take cautiously,” she said. “There is a reason why we haven’t had active COVID at Shepherd Village and if we cast aside all of the precautions, it would have made no sense to work so hard to keep our residents safe up to this point. That said, there are stages and our first step is just taking the residents outside for an hour or so to get some fresh air. We haven’t found a way as yet to integrate families. We had issues with the palliative visits where there was a person who refused to stay in the room with his loved one and was seen walking through our hallways with mask in his hand, saying ‘he’s tired of this hot thing on his face’. Our staff was literally in tears because it only takes one person to undo all the hard work.
“We also know that when families are reunited with their loved ones, there might be the urge to hug them. We are thinking about what we can do to facilitate visits and how we can do it safely. At the moment, we are working with the Family Council to come up with some ideas. They have said people will be screened and they will have to wear PPEs which is a cost if I have to provide for family members to come in. We are looking at staggering visits for each floor during the day and there will have to be a staff member with each resident to ensure that families are respecting the rules. We are also thinking about doing the visits outside in the garden.”
Beckles said Shepherd Village will be vigilant and on high alert until a vaccine is developed.
“The virus is invisible and it could walk in here today or tomorrow,” she noted. “We still have to be prepared and follow all of the necessary protocols. I believe that COVID is here to stay in a way that we can’t just go back to being blind to the possibility of infection, Today, it’s COVID and down the road it might be something worse. Also, the vaccine wouldn’t have had three years of trial, so we don’t know what will be the repercussions of taking it too soon.”
Opened in 1961 after being incorporated three years earlier as the Pentecostal Benevolent Association of Ontario, Shepherd Village – which subsidizes its long-term care up to $1 million annually as it only receives operational funding from the provincial government for that segment -- meets the physical, spiritual, emotional and social needs of individuals seeking assistance in a Christian environment.
Its continuum of care concept offers five distinct styles of senior living.
In her role, Beckles is responsible for governance, operations, client care, community relations and business development.
She joined Shepherd Village in January 2017 after spending 14 years as Chief Financial Officer (CFO) and Vice-President of Kensington Health Centre which is a 350-bed long-term residential hospice.
“Working at Kensington was my first introduction to health and seniors care and there’s a lot of compassion and patience I learned working with the elderly,” said Beckles who co-founded the Leadership, Empowerment, Achievement and Determination (LEAD) program which provides newcomers and struggling high school students with life skills and helps them make a seamless transition to tertiary level education.
“As I walk the Village here now that I am in charge and I see the eyes of seniors looking at me just literally saying, ‘I know you are going to keep us safe’, there’s a heavy burden knowing you have all of these people who are frail and are counting on you to make decisions that will keep them safe. Dealing with a vulnerable population and understanding you can’t wait for governments to step up and give you the money you need are also things I grasp. Long-term care has always been underfunded and I know this because I dealt with the numbers when I was the CFO at Kensington.”
Wendy Beckles (r) co-founded the LEAD program with Catherine Bruce (l), Nicole Baxter and Dr. Juliet Daniel
The product of a Barbadian father and Vincentian mother, Montreal-born Beckles spent almost 12 years in Barbados and four in Ghana – where her dad, Archibald Rowe, taught Math – before returning to Canada in 2000 with her husband, Mark Beckles, who is RBC’s Senior Director of Youth Strategy & Innovation.
She was with International Child Care as an International Financial Controller for three years before joining Kensington.